1. Introduction
Acinetobacter baumannii has, over the past few decades, shifted from relative obscurity to near notoriety in hospital settings. What makes this organism particularly alarming is not simply its persistence in intensive care units, but its capacity to combine multidrug resistance with an increasingly aggressive virulence profile (Bush & Bradford, 2020). This dual threat has complicated treatment strategies and intensified global concern.
Initially regarded as a low-grade opportunistic pathogen, A. baumannii has demonstrated remarkable genomic adaptability. Regulatory mechanisms, including global transcriptional regulators such as H-NS, contribute to the modulation of virulence-associated traits and environmental responsiveness (Eijkelkamp et al., 2013). Such regulatory flexibility enables the bacterium to coordinate stress adaptation, biofilm formation, and resistance expression in response to antimicrobial exposure.
Clinically, infections caused by hypervirulent strains extend beyond typical opportunistic presentations. Severe pneumonia, bloodstream infections, and device-associated infections are increasingly reported, particularly in critically ill individuals. Host vulnerability plays an important role; impaired immune or hematologic status can heighten susceptibility to invasive bacterial infections (Abuga et al., 2020). This interaction between host susceptibility and bacterial adaptability underscores the complexity of hvAB pathogenesis.
A defining feature of hypervirulent A. baumannii is its ability to adhere to surfaces and form resilient biofilms. The structural and functional assembly of adhesive organelles has been extensively characterized in other Gram-negative pathogens (Chahales & Thanassi, 2015). Specific adhesion molecules such as FimH in uropathogenic bacteria illustrate how surface proteins contribute to colonization and persistence within host tissues (Chen et al., 2009). In A. baumannii, analogous adhesive mechanisms support colonization of both host epithelia and abiotic medical devices.
Biofilm formation further enhances tolerance to antimicrobial agents and environmental stressors. Emerging antibacterial materials and surface-modifying strategies have been proposed as innovative tools to counteract biofilm-associated pathogens (Ding et al., 2018). Additionally, anti-adhesive compounds such as ceragenins have shown promise in reducing A. baumannii colonization and biofilm development (Karasinski et al., 2024). Together, these findings emphasize the importance of targeting adherence and biofilm integrity in hvAB management.
Iron acquisition is another critical determinant of virulence. Hosts actively restrict iron availability as part of nutritional immunity, limiting microbial growth. Siderophore systems play a central role in overcoming this barrier. The broader significance of siderophores in microbial physiology and virulence has been well established (Haas et al., 2008), while classic studies in Escherichia coli highlight enterobactin-mediated iron uptake as a model system (Hantke, 1990). Disrupting iron metabolism represents a promising therapeutic strategy; for example, gallium nitrate has demonstrated both in vitro and in vivo activity against multidrug-resistant A. baumannii by interfering with iron-dependent processes (Antunes et al., 2012).
Interestingly, host-derived iron-binding proteins such as lactoferrin also influence microbial survival. Clinical investigations into lactoferrin supplementation have demonstrated antimicrobial-modulating effects in other bacterial infections (Di Mario et al., 2003; Di Mario et al., 2006). These findings raise the possibility that manipulating iron availability may serve as an adjunctive strategy in hvAB infections.
The mechanisms underlying bacterial killing by antibiotics remain an area of debate. While reactive oxygen species (ROS) were once considered central to bactericidal activity, evidence suggests that antibiotic-mediated killing does not universally depend on ROS generation (Keren et al., 2013). Nonetheless, reactive oxygen species themselves possess antimicrobial properties and have been explored as alternative therapeutic approaches (Dryden, 2018). Understanding these mechanisms is essential for refining strategies against highly resistant pathogens.
Beyond resistance, structural adaptations also contribute to antimicrobial tolerance. For example, cell wall thickening has been identified as a resistance mechanism in other Gram-positive bacteria (Cui et al., 2003). Although the molecular architecture differs in Gram-negative organisms, analogous structural modifications may influence permeability and drug susceptibility in A. baumannii.
Given the increasing limitations of conventional antibiotics, newer pharmacologic agents are being evaluated. The phase 3 ATTACK trial demonstrated that sulbactam–durlobactam was non-inferior to colistin for serious infections caused by the A. baumannii–calcoaceticus complex, with improved safety outcomes (Kaye et al., 2023). Such findings represent meaningful progress, although vigilance is required to monitor emerging resistance.
In parallel, immunization and host-directed strategies are gaining traction. Conjugate vaccines targeting siderophores have successfully reduced intestinal colonization by pathogenic bacteria in animal models (Cui et al., 2020). Multivalent vaccine formulations incorporating novel antigens have also elicited broad protection against bacterial infections (Deng et al., 2019). More recently, vaccination-induced innate immune training has demonstrated rapid protective effects against bacterial pneumonia in experimental systems (Gu et al., 2021). These immunological approaches suggest that augmenting host defenses may complement antimicrobial therapy.
Collectively, the evolving landscape of hypervirulent Acinetobacter baumannii highlights a convergence of resistance, virulence, and adaptive regulation. The pathogen’s capacity to acquire ß-lactamases and other resistance determinants continues to complicate therapeutic decision-making (Bush & Bradford, 2020). At the same time, emerging perspectives emphasize the importance of protective strategies that bridge the gap between infection onset and microbial eradication (Gal et al., 2023).
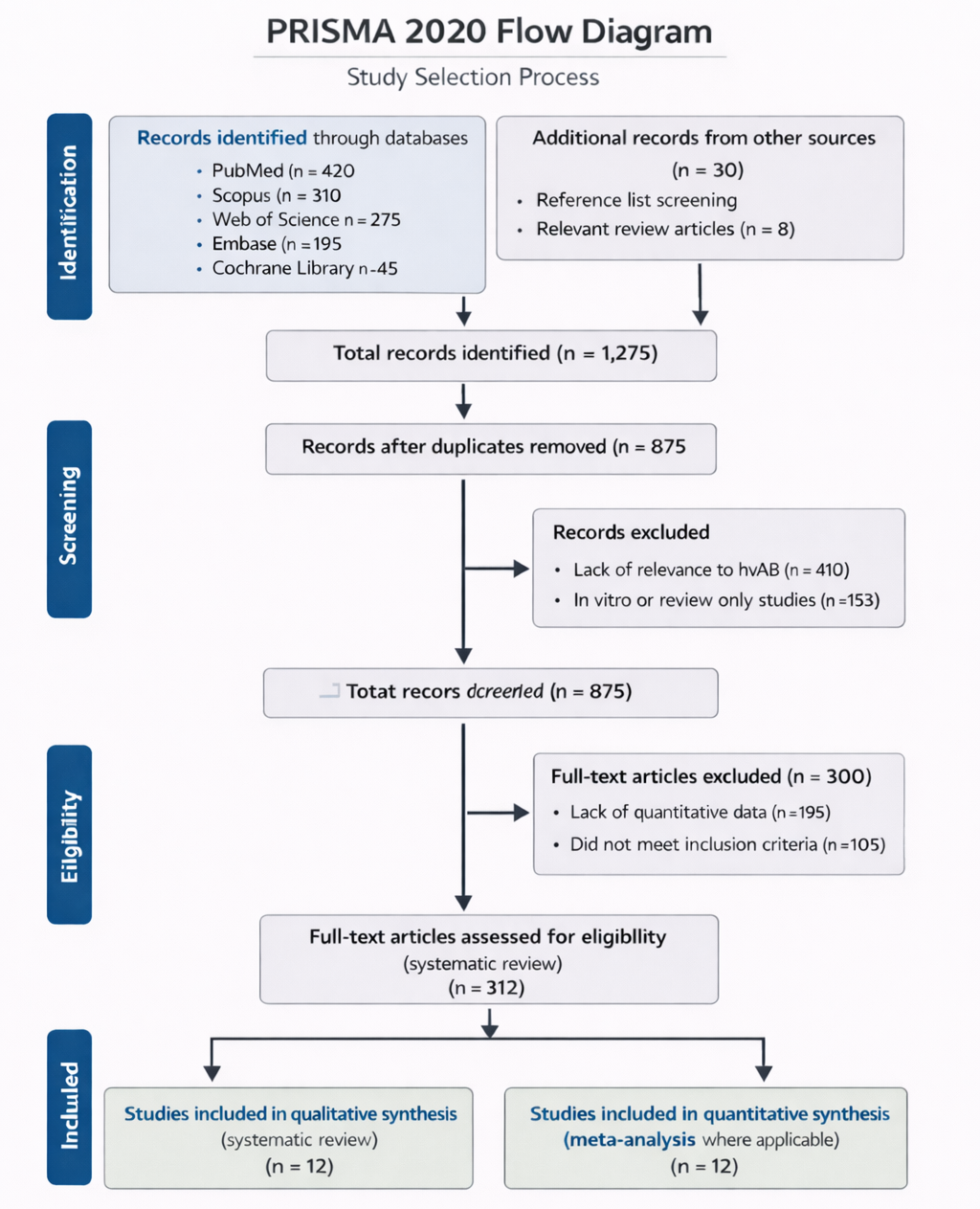
Despite expanding research, evidence remains dispersed across molecular studies, clinical trials, and experimental models. A comprehensive synthesis integrating virulence determinants, antimicrobial resistance mechanisms, and emerging therapeutic strategies is therefore essential. This systematic review and meta-analysis aim to consolidate current knowledge, quantify the contribution of key virulence mechanisms, and evaluate evolving treatment approaches against hypervirulent, multidrug-resistant A. baumannii.